Combined Modalities for HDR and IMRT
Treatments of Prostate Cancer
Jack Yang,
Ph.D, Sang
Purpose: To evaluate the clinical benefits when applying both
High Dose Rate (HDR) brachytherapy and IMRT external beam treatment for
intermediate and high risk prostate cancer patients. By properly managing the
treatment schemes, we can easily achieve the optimum dose distribution while
maintaining very low dose to critical organs which might translates to low risk
of complication for rectum and urethra.
Method and Materials: HDR brachytherapy
has several potential advantages, in terms of the ability to control the
implant quality (may be related to the local control probability). HDR brachytherapy applies advanced technology to delivery optimized dose
distribution of Ir-192. It allows the user to modulate the intensity of the
radiation by varying the dwell time of the source within the implant. By
changing the dwell time during the planning process, not only the hot and cold
spots in the prostate can be reduced to an acceptable level, but also can
improve the uniformity dose distribution to the peripheral zone of the prostate
PTV. If planned accordingly, the bulky cancer area is also possible to accept
higher doses to elevate the radiation to the disease site (non-uniform or
differential dose distribution). HDR treatment provides an alternative to the
current prostate treatment with efficiency and potential clinical benefits.
Patient selection criteria at MMC is as follows: 1) PSA > 10; 2) Gleason
7-10; 3) Bulky T2a or ≥T2b; 4) Positive nodal involvement; 5) 4 cores and/or
bipolar disease; 6) Negative met work-up. Combined with IMRT external beam
treatment, this technique creates a superior dose distribution for intermediate
and high risk prostate cancers. The main differences compared to other
treatment modalities are the high dose rate and the fractionation. We designed
and applied a fractionated dose protocol from linear-quadratic calculations
that we believed was comparable to continuous low-dose-rate brachytherapy, this
bring the dose comparison to the common ground. The HDR
treatment fraction at MMC is 7Gy x3 then followed with the IMRT treatment for
50Gy, biologically, it is equivalent to about the range of 86 Gy. With this
dose level, from our clinical data which presents low level of complication and
comparable survival rate to patients who received IMRT treatment, we believed
that the dose is high enough to generate acceptable clinical benefits. Fig. 1
shows the CT scout view for the needle tip identification, and Fig. 2 indicates
the need pattern on the axial view for needle pattern for urethra and rectum
sparing.
Results: Most of the reported HDR results with prostate
cancer involve combination of IMRT, preceding or followed with an HDR boost,
present excellent clinical results. For the past 6 years, we have treated more
than 1000 patients with this type of treatment regiment with HDR and IMRT
combination. Clinical data indicated much better and/or reduced complication
rate compared to the single modality either with IMRT or seed implant technique
alone (for intermediate and high risk prostate patients). Since dose
distribution can be manually adjusted in the planning process for the best
coverage for PTV and sparing of the rectum, most importantly, the urethra
complication has been greatly reduced since we have the capability to control
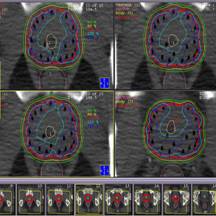
the hot spot close to the urethra area. Fig. 3 Sows excellent coverage on PTV
while the 125% Isodose line spare the urethra and rectum completely. This is
one of the typical cases for prostate HDR treatment at MMC.
Conclusion: HDR plus the IMRT external beam treatment provides
another great methodology to eradicate the prostate cancer. With the successful
clinical implementation, our patients received the most advanced techniques in
the department. The long term survival outcome will be analyzed completely in
the next few years.
Fig. 3 An
optimized dose distribution, with 125% isodose lines spared urethra and
rectum Fig. 2 Needle pattern for a typical case Fig. 1 Sagittal view of needle implant